VIROLOGY OF HCV
Chronic infection with the hepatitis C virus (HCV) is relatively frequent and widespread through the world. Chronic hepatitis C has become recognized as a significant public health problem both in developed Western countries and around the world. For example, in the USA it is the single biggest indication for liver transplantation and accounts for more than 10 000 deaths each year.
There is also growing public awareness of hepatitis C and its complications.
This growing awareness of hepatitis C has led to greater efforts by public health authorities to develop effective strategies to control HCV infection and its complications. In 2002, a National Institutes of Health Consensus Development Conference was held on the management of hepatitis C in Bethesda, Maryland. The proceedings of that meeting were summarized in a Consensus Statement which forms a valuable resource in the management of hepatitis C.
BACKGROUND
Although it had been recognized for several years that certain forms of hepatitis could be transmitted parenterally, it was only after the discovery of the viral agents responsible for hepatitis B and hepatitis A and serologic tests for these agents that it became apparent some cases of blood-borne hepatitis were due to another agent (referred to as non-A, non-B hepatitis). Many characteristics of the clinical features and natural history of non-A, non-B hepatitis were elucidated by studying cases of post-transfusion hepatitis by monitoring serum aminotransferase activities and liver histology.
The agent responsible for parenteral non-A, non-B hepatitis was discovered using the techniques of molecular biology and cloning by Houghton and co-workers at Chiron Corporation who cloned a fragment of the hepatitis C virus in an expression vector. The cloned fragment was then detected by reaction with antibodies present in human serum from individuals infected with HCV. This landmark discovery led to the development of a diagnostic assay for antibodies to HCV and was followed by full-length cloning of the virus. Polymerase chain reaction (PCR)-based assays to detect the viral genome allowed further clarification of the natural history and epidemiology of hepatitis C.

Even before the discovery of HCV several investigators had tested interferons as therapy for chronic non-A, non-B hepatitis. These early studies indicated that interferon therapy was associated with suppression of serum aminotransferase activities, albeit often transient. Considerable progress has since been made in developing effective therapies against hepatitis C.
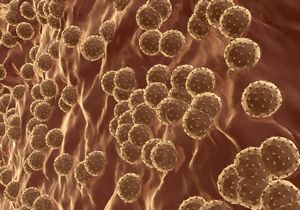
HCV is a single-stranded RNA virus belonging to the family Flaviviridae. Its genome is approximately 10 000 nucleotides in length and consists of a single open reading frame (ORF) with non-coding RNA regions at its 5' and 3' ends. The single ORF codes for one large protein which is then cleaved into a series of smaller proteins by viral and host proteases.
These smaller proteins constitute the structure of the virus (structural proteins: core, E1 and E2) or form part of the replicative machinery of the virus (the non-structural proteins: NS2, NS3, NS4 and NS5). Both the 5' and 3' non-coding regions of the viral genome appear to be critical to its function. The 5' non-coding region serves as an internal ribosomal entry site (IRES) which binds to cellular ribosomes and facilitates the production of viral proteins.
Although the exact function of the 3' end is uncertain, HCV cannot replicate effectively in its absence.
The RNA genome of HCV replicates through an RNA-dependent RNA polymerase (RdRp) coded for by the NS5B gene of HCV. The RNA genome of HCV is very prone to mutation resulting in considerable variability in its RNA sequence. Based on differences in RNA sequence, six major genotypes of HCV have been identified with multiple subtypes. Isolates from individual patients also contain a quasispecies 'swarm' of closely related but distinct viral sequences.
HCV genotypes have been of interest from an epidemiologic point of view as they have allowed study of HCV in various populations. Some genotypes are confined to or found largely in certain geographic areas -for example, HCV genotype 5 in southern Africa, genotype 4 in Egypt and the Middle East and genotype 6 in south-east Asia. Genotypes 1, 2 and 3 are found in developed Western countries, Japan and Australia in various proportions. Interestingly, HCV genotype also seems to affect the biologic behavior of the virus with regard to response to antiviral therapy -those patients infected with HCV genotypes 2 or 3 respond much better to interferon-based therapies than those with HCV genotype 1.
HCV is a largely hepatotropic virus that replicates only in humans and certain non-human primates such as chimpanzees and tamarins. These features have made it difficult to grow reliably in cell culture, thus hampering research into its repli-cation and the development of new therapeutic agents. HCV has been reported to grow at low levels in certain lymphocytoid and hepatic cell lines.
More recently, researchers have relied on a replicon system which utilizes an artificial construct of non-structural chimeric HCV genes in a cell line derived from hepatocellular carcinoma (HCC). Relatively high levels of HCV replication have been observed in the replicon system and it seems a suitable model for studying the effects of antiviral drugs. Nonetheless this system is limited because only certain genotypes of HCV replicate effectively and the structural proteins of HCV are not produced.
A reliable small animal model for HCV propagation has only recently been developed. The chimpanzee has been the best animal model for HCV infection and disease. However, as the use of chimpanzees is extremely expensive, it is not at all practical for most studies of HCV replication to be performed in chimps.
Recently HCV replication in transgenic mice chimeric for human livers was described. This system uses SCID/beige mice crossed with mice carrying a plasminogen activator transgene, urokinase plasminogen activator, under the control of the albumin promoter (Alb-uPA). The transgene leads to accelerated mouse hepatocyte death conferring a replicative advantage for transplanted hepatocytes that lack the uPA transgene.
In this application the transplanted hepatocytes could be derived from either humans or chimpanzees. Back-crosses are required to generate mice homozygous for both the SCID trait and the Alb-uPA. Mercer et al (01). demonstrated infection of transplanted mice with HCV in the doubly homozygous animals and transient replication of HCV in the hemizygous animals using human hepatocytes.

 RSS Feed
RSS Feed
